- May 11, 2008
- 23,272
- 1,573
- 126
Alzheimer's disease and the HVS1.
This option has been researched since 1988 and more and more prove stacks on that this is the case since the last 20 years.
http://www.nytimes.com/1988/07/23/us/research-suggests-virus-link-to-alzheimer-s-disease.html
http://www.sciencedaily.com/releases/2008/12/081207134109.htm
http://brainblogger.com/2010/12/15/alzheimer’s-disease-vaccine-on-the-horizon/
This option has been researched since 1988 and more and more prove stacks on that this is the case since the last 20 years.
http://www.nytimes.com/1988/07/23/us/research-suggests-virus-link-to-alzheimer-s-disease.html
http://www.sciencedaily.com/releases/2008/12/081207134109.htm
They believe the herpes simplex virus is a significant factor in developing the debilitating disease and could be treated by antiviral agents such as acyclovir, which is already used to treat cold sores and other diseases caused by the herpes virus. Another future possibility is vaccination against the virus to prevent the development of the disease in the first place.
Alzheimer's disease (AD) is characterised by progressive memory loss and severe cognitive impairment. It affects over 20 million people world-wide, and the numbers will rise with increasing longevity. However, despite enormous investment into research on the characteristic abnormalities of AD brain - amyloid plaques and neurofibrillary tangles - the underlying causes are unknown and current treatments are ineffectual.
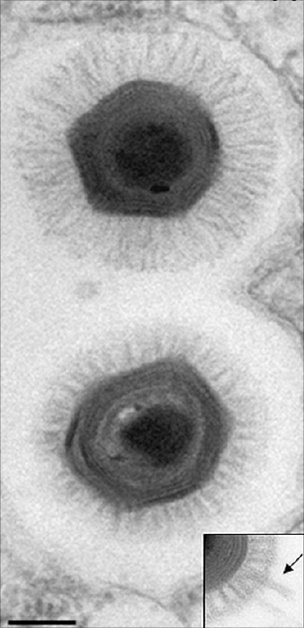
Professor Ruth Itzhaki and her team at the University's Faculty of Life Sciences have investigated the role of herpes simplex virus type 1 (HSV1) in AD, publishing their very recent, highly significant findings in the Journal of Pathology.
Most people are infected with this virus, which then remains life-long in the peripheral nervous system, and in 20-40% of those infected it causes cold sores. Evidence of a viral role in AD would point to the use of antiviral agents to stop progression of the disease.
The team discovered that the HSV1 DNA is located very specifically in amyloid plaques: 90% of plaques in Alzheimer's disease sufferers' brains contain HSV1 DNA, and most of the viral DNA is located within amyloid plaques. The team had previously shown that HSV1 infection of nerve-type cells induces deposition of the main component, beta amyloid, of amyloid plaques. Together, these findings strongly implicate HSV1 as a major factor in the formation of amyloid deposits and plaques, abnormalities thought by many in the field to be major contributors to Alzheimer's disease.
The team had discovered much earlier that the virus is present in brains of many elderly people and that in those people with a specific genetic factor, there is a high risk of developing Alzheimer's disease.
The team's data strongly suggest that HSV1 has a major role in Alzheimer's disease and point to the usage of antiviral agents for treating the disease, and in fact in preliminary experiments they have shown that acyclovir reduces the amyloid deposition and reduces also certain other feature of the disease which they have found are caused by HSV1 infection.
Professor Itzhaki explains: "We suggest that HSV1 enters the brain in the elderly as their immune systems decline and then establishes a dormant infection from which it is repeatedly activated by events such as stress, immunosuppression, and various infections.
http://brainblogger.com/2010/12/15/alzheimer’s-disease-vaccine-on-the-horizon/
HSV1 is ubiquitous, identified in approximately 90% of adults. Normally, an infection with HSV1 occurs in infancy, but the virus remains lifelong in the peripheral nervous system in a latent, inactive state. HSV1 can be reactivated later in life by stress, immunosuppression, fever or ultraviolet light exposure; HSV1 is the virus that causes cold sores. Researchers postulate that if HSV1 reaches the brain, the virus could cause damage consistent with AD. Likewise, HSV1 is already identified as the cause of herpes simplex encephalitis, a rare but serious brain disorder, which leaves survivors with memory loss and a loss of cognitive function, just as AD does.
HSV1 does not cause AD on its own. There are likely host factors that alter the risks for developing AD. Interestingly, a genetic component — the type 4 allele of the apolipoprotein E gene, which normally transports lipids in the body and repairs tissue damage — confers a high risk of AD when associated with HSV1. (The same genetic component is an increased risk factor for cold sores.)
Two hallmarks of AD are the presence of amyloid plaques and neurofibrillary tangles in the brain. Beta-amyloid, the primary component of the plaques, accumulates in the presence of HSV1 infections. Further, 90% of plaques evaluated from AD brains contained HSV1, and 72% of the virus DNA was associated with plaques; in normal, aged brains, which contain amyloid plaques at a much lower frequency than AD brains, 80% of the plaques contained HSV1, but only 24% of the viral DNA was plaque-associated. In normal brains, it is likely that there is a lesser production or greater removal of beta-amyloid, so it is less likely that HSV1 would be able to interact destructively inside the brain. Basically, HSV1 infection likely induces changes in gene expression in the brain, through its inflammatory and oxidative processes, that are damaging to the brain.
The only current pharmacological therapies approved for AD are acetylcholinesterase inhibitors and N-methyl-D-aspartic acid receptor inhibitors, which demonstrate symptomatic improvement, but do not treat the underlying cause of AD. The proposed involvement of HSV1 in AD has led to the possibility of the first potentially disease-modifying treatments in AD. Antiviral agents, such as acyclovir and valacyclovir, may be beneficial in preventing disease progression in AD patients. These agents inhibit the synthesis of viral DNA, preventing its spread throughout the body and the damage it causes. (Acyclovir is also being evaluated in the treatment of multiple sclerosis, owing to another herpes virus implicated in the development of that disease.) Alternatively, a vaccine to prevent the reactivation of HSV1 and prevent AD altogether is being evaluated in human trials. Anti-viral agents are the first attempt to prevent the pathogenesis of AD, rather than just treat the symptoms, offering hope to millions of current and future AD sufferers and their families.
Chackerian B (2010). Virus-like particle based vaccines for Alzheimer disease. Human vaccines, 6 (11) PMID : 20864801
Chackerian B, Rangel M, Hunter Z, & Peabody DS (2006). Virus and virus-like particle-based immunogens for Alzheimer’s disease induce antibody responses against amyloid-beta without concomitant T cell responses. Vaccine, 24 (37-39), 6321-31 PMID : 16806604
Hill JM, Zhao Y, Clement C, Neumann DM, & Lukiw WJ (2009). HSV-1 infection of human brain cells induces miRNA-146a and Alzheimer-type inflammatory signaling. Neuroreport, 20 (16), 1500-5 PMID : 19801956
Itzhaki RF, & Wozniak MA (2006). Herpes simplex virus type 1, apolipoprotein E, and cholesterol: a dangerous liaison in Alzheimer’s disease and other disorders. Progress in lipid research, 45 (1), 73-90 PMID : 16406033
Lukiw WJ, Cui JG, Yuan LY, Bhattacharjee PS, Corkern M, Clement C, Kammerman EM, Ball MJ, Zhao Y, Sullivan PM, & Hill JM (2010). Acyclovir or Abeta42 peptides attenuate HSV-1-induced miRNA-146a levels in human primary brain cells. Neuroreport, 21 (14), 922-7 PMID : 20683212
Sabbagh, M., & Berk, C. (2010). Latrepirdine for Alzheimer’s disease: trials and tribulations Future Neurology, 5 (5), 645-651 DOI: 10.2217/fnl.10.53
Wozniak MA, Mee AP, & Itzhaki RF (2009). Herpes simplex virus type 1 DNA is located within Alzheimer’s disease amyloid plaques. The Journal of pathology, 217 (1), 131-8 PMID : 18973185
Wozniak, M., & Itzhaki, R. (2010). Antiviral agents in Alzheimer’s disease: hope for the future? Therapeutic Advances in Neurological Disorders, 3 (3), 141-152 DOI: 10.1177/1756285610370069